ENDOMETRIOSIS
What is Endometriosis?
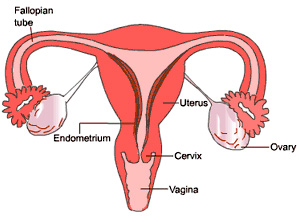
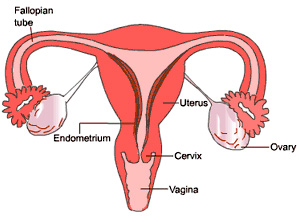
Endometriosis is a disease characterized by the presence of tissue which is histologically identical to endometrium (the inner lining of the uterine wall) outside the uterine cavity. Usually, endometriosis is confined to the pelvic and lower abdominal cavity; however, it has occasionally been reported to be in other areas, as well.
Endometriosis is one of the most common problems that gynecologists currently face. It is one of the most complex and least understood diseases in our field and, despite many theories, we still do not have a clear understanding of the cause or of its relationship to infertility. Since this disorder is primarily a human disease and rare in other animal species, accumulation of the facts has been slow.
Although endometriosis has been considered a pathological or separate disease entity, it may not be a disease at all. It may actually be the clinical manifestation of a more basic underlying disorder, such as a basic chemical or physiological abnormality that affects the tubal motility or immune system which could be responsible for the initiation or progression of endometriosis in patients with retrograde menstrual flow. By the same token, endometriosis may not be the cause of infertility, but the result of it. Historically, it has been shown that sometimes our understanding of a disease has awaited the technology to explain it. This may very well be the case with endometriosis, especially in regard to its immunological aspects. Further technological developments may be necessary in order for us to fully understand this problem.
How common is Endometriosis?
In literature, the prevalence of this disease in the general population has been reported to be about five percent of the female population of reproductive age. However, in women with severe menstrual cramps, the incidence of endometriosis has been reported to be between 25 and 35 percent.
Is there any age group which is more prone to endometriosis?
Endometriosis has been reported only in the reproductive ages, which means right after the start of the menstrual cycle until menopause or immediate post-menopausal years.
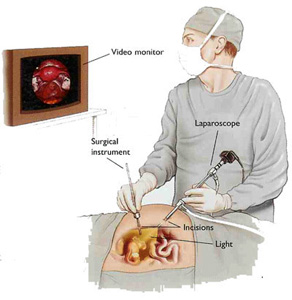
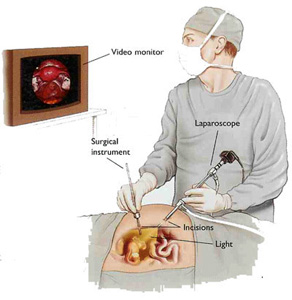
We believe that ovarian function is necessary for the development and maintenance of these endometrial implants. The disease is normally not seen before age 15 or after menopause. In recent years, we have seen more patients with endometriosis below the age of 20. This is due to the use of laparoscopy in evaluating women with symptoms suggestive of endometriosis.
In a recent study of 140 patients aged 10.5 years to 19 years who were complaining of severe pelvic pain, 47 percent had documented endometriosis at laparoscopy as the sole reason for their pelvic pain.
Is endometriosis based on a genetic or familial factor?
Several studies have shown that the incidence of endometriosis is much higher in women having a sister or mother who has already had endometriosis. There was a study conducted involving more than 150 women with endometriosis; of these, 18 (12 percent) were found to have a mother or sister with endometriosis. However, in the same group of women, only two (1.5 percent) showed that they had a mother-in-law or sister-in-law who had endometriosis. This clearly shows that there is a familial tendency with endometriosis. As one can see from these figures, there is almost an eight-fold increase in the risk of endometriosis in women whose mother or sister has been diagnosed as having the disease.
Equally important was the finding that endometriosis on a familial basis tended to be at a more advanced stage when diagnosed and also that it acts more aggressively. It has been suggested that endometriosis might result from an inheritable immunodeficiency state.
Is it true that women who have their tubes tied are protected against endometriosis?
Theoretically, blockage of the tubes by tubal ligation or by any other cause (for instance, pelvic inflammatory disease) should protect against the further production of endometriosis. However, a recent investigation of women requesting tubal ligation reversal has not supported this concept. The prevalence rates for endometriosis were found to range from 2 percent through 12 percent in two studies. When an infertile population is studied, these rates range from 5 percent through 35 percent.

Is it true that intercourse during the menstrual cycle increases the risk of endometriosis?
This has not been proved. It has been suggested that intercourse during menses might increase tubal activity and increase the backflow of the menstrual cycle through the tubes and thus increase the risk of endometriosis. However, there are no statistics to bear this out.
At the time of my laparoscopy, my doctor was not able to get a biopsy. Is the physical appearance of endometriosis adequate for diagnosis?
A biopsy of the lesion does document the presence of endometrial tissue. I believe that the gross appearance of endometriosis and visual inspection of the pelvis is adequate and accurate for diagnosis of endometriosis. However, before any treatment starts, the diagnosis should be confirmed by visual inspection. In a recent study in 86 patients with a visual diagnosis via laparoscopy, diagnosis was confirmed in 93 percent by biopsy. However, in those cases that were believed not to have endometriosis by visual inspection, only 6 percent had a tissue diagnosis of endometriosis confirmed.
It is also important that the surgeon you select is well educated in the appearance of endometrial lesions. Today, many surgeons will videotape the laparoscopy and this can be reviewed at a later date if there are any questions.
Why does endometriosis seem to be discussed more in recent years?
Endometriosis is one of the most common gynecological diseases and is responsible for a significant portion of gynecological surgeries each year. Almost as important as the numbers is the fact that young women with endometriosis are often faced with difficult decisions regarding their future reproduction. One of the main symptoms or consequences of endometriosis is infertility, and since there has been a renewed interest in the United States in fertility, there has also been a renewed interest in this disease. The introduction of the laparoscope for more accurate diagnosis of endometriosis has also helped us to diagnose more cases in earlier stages in younger women. The result of this increased attention is that more and more women are now forewarned about the symptoms of the disease.
Is it true that endometriosis is more common in some races?
There seems to be some evidence among researchers that Caucasian women are at greater risk than blacks. Two studies have found the prevalence of endometriosis in blacks to be half that of whites. However, the notion that black women rarely suffer from endometriosis is incorrect. Some data shows that the risk of disease among Asian women is even higher than in Caucasians. There are also several studies which suggest that this disease is more common among higher socio-economic groups of women.
Is there a characteristic menstrual cycle of the woman who has endometriosis?
Yes. Many studies have shown that women with endometriosis begin their menstrual cycle at a significantly younger age than women without the condition. Endometriosis is more prevalent in women who have a regular cycle than in women who have an irregular cycle. Another interesting characteristic is that patients with endometriosis have a shorter interval between their periods (less than 27 days). Severe menstrual cramps are also seen much more frequently in endometriosis.
It has been shown that the chance of having endometriosis is four times greater in patients with severe menstrual cramps as compared to women with mild menstrual cramps. Another point is that patients with a prolonged menstrual flow are apt to have endometriosis. It has also been found that if the menstrual flow is longer than a week, the risk of developing endometriosis is 2.5 times greater than in women who have a menstrual flow lasting less than a week.
It has been suggested that the total bulk of endometrial cells cast into the peritoneal cavity may be a factor. Women with a greater number of menstrual days (a factor of days of flow and cycle interval) had twice the risk of developing endometriosis.
Is there a characteristic menstrual cycle of the woman who has endometriosis?
Yes. Many studies have shown that women with endometriosis begin their menstrual cycle at a significantly younger age than women without the condition. Endometriosis is more prevalent in women who have a regular cycle than in women who have an irregular cycle. Another interesting characteristic is that patients with endometriosis have a shorter interval between their periods (less than 27 days). Severe menstrual cramps are also seen much more frequently in endometriosis.
It has been shown that the chance of having endometriosis is four times greater in patients with severe menstrual cramps as compared to women with mild menstrual cramps. Another point is that patients with a prolonged menstrual flow are apt to have endometriosis. It has also been found that if the menstrual flow is longer than a week, the risk of developing endometriosis is 2.5 times greater than in women who have a menstrual flow lasting less than a week.
It has been suggested that the total bulk of endometrial cells cast into the peritoneal cavity may be a factor. Women with a greater number of menstrual days (a factor of days of flow and cycle interval) had twice the risk of developing endometriosis.
Is there a relationship between endometriosis and the use of tampons?
This is unlikely. Scientifically, there has not been any basis to conclude that the use of tampons increases the risk of developing endometriosis. Also, with regard to other hygienic practices (such as douching after the menstrual period), it has not been shown that this increases the risk of endometriosis.
Do women with more menstrual cramps have a greater tendency to acquire endometriosis?
Although one of the most common characteristics of women with endometriosis is severe menstrual cramps, this appears to be the result of the disease rather than a precursor to it.
If I put off having children until my 30s or later, do I have a greater chance of getting endometriosis? Also, is there any truth to the belief that delayed childbirth can lead to endometriosis?
This theory first surfaced in the early 1950s along with the idea that early childbearing offered protection against endometriosis. Although the incidence of endometriosis is higher in women who delay having their first child, this may be because of the fact that endometriosis causes infertility. It is therefore difficult to distinguish whether the infertility preceded or followed the endometriosis. We do believe, however, that pregnancy does have a protective effect on women with endometriosis.
I have heard that career women have a higher chance or risk of developing endometriosis. Is there any truth to this?
At the present time there is no scientific justification that supports this theory, and it is more of a myth than a fact that endometriosis is primarily a disease of thin, Caucasian, career women with compulsive personalities.
Although there are studies that show women who exercise regularly had a lower risk of developing endometriosis than women who did not, the protective effect appeared to be confined to women who had begun their activity at an early age and who exercise more than two hours weekly. The types of activity most likely associated with decreased risk were conditioning exercises such as jogging. It is presumed that exercise may influence the risk of this disease through its effect on the level of hormones, such as estrogen, in the women's bodies.
My mother used DES while she was pregnant with me. Does this use of DES in utero increase the risk of endometriosis?
At the present time, there is no clear study which can relate an increase in endometriosis incidence with DES exposure.
Are you seeing more endometriosis in younger women today?
We are diagnosing this disease right now in a younger age group of women. Twenty-five years ago, our diagnosis was mainly based on severe symptoms and palpable masses in the pelvic area, and was confirmed by laparotomy. Patients were typically in their mid or late 30s. However, with the use of laparoscopy, the typical age at which the diagnosis is being made has dropped significantly. Currently, it is somewhere in the mid to late 20s. We are expecting a further decline in the average age of diagnosis because of the added knowledge of the disease in younger women and also the availability and increased use of laparoscopy in confirming diagnosis.
Do you see endometriosis after menopause?
Normally, no. This is because the growth of endometrial implants are dependent upon the female hormone. After menopause, the ovaries cease to produce the hormones that promote the growth of endometriosis and we usually do not see many cases. However, after menopause, there are two factors which may promote or maintain endometriosis. One is the use of estrogen replacement therapy and the other is the presence of high endogenous estrogen in obese patients.
Is endometriosis a disease of modern times?
The presence of endometrial tissue outside the uterus was first reported about 300 years ago in 1696 by Sabiard. However, since the turn of the century, and especially in the 1920s, it has been known that endometrial tissue outside of the uterus is responsible for painful menstruation, pelvic pain, pain with intercourse and infertility. The fact that we have been hearing more about endometriosis in the past two or three decades is, I think, due to more awareness by the public and physicians about the condition.
Today, physicians are looking more for this condition in patients who have pelvic pain, pain with menstruation and infertility. Also, there are better tools for diagnosing endometriosis, especially in the early stages. The primary tool was once only the pelvic examination, or at the time of surgery. However, with the use of laparoscopy, we are diagnosing this disease in women in earlier stages who have the above-mentioned symptoms

What does endometriosis look like?
The presence of endometriosis is characterized by blue-gray lesions on the peritoneal surface, over the pelvic peritoneum or pelvic structures. This distinct appearance can be attributed to the encapsulated menstrual blood and menstrual debris. However, the appearance is critically dependent upon the longevity of the tissue implanted. The initial appearance may be just an irregularity or discoloration of the peritoneal surface. Initially, these lesions may appear tan or hemorrhagic in color. After establishment of viable endometrial transplant and menstrual shedding, the presence of entrapped menstrual debris gives the tissue the typical blue-gray and powder burn appearance.
Many times the lesion of endometriosis may not have any color at all. These lesions are called nonpigmented endometriosis. Many experts believe that a young patient or a patient in the reproductive ages (15 to 50) who has an area on the peritoneal surface that does not look normal, and who is having symptoms of endometriosis (i.e., pelvic pain, pain with periods or intercourse, and infertility), should be considered as having endometriosis until it is proven otherwise.
Clinically, these early lesions, although less impressive than pigmented ones when viewed laparoscopically, are just as important in producing pain and infertility.
What are the most common symptoms of endometriosis?
The symptoms of endometriosis may be highly variable from one patient to another. The magnitude of the symptoms may not correlate with the extent of the disease, either. For example, a patient with severe disease may have very little pain. However, the likelihood of infertility does increase as the severity of the disease increases. The clinical presentation and symptoms of the disease are also frequently related to the anatomical site of the disease.
The most common sites of the disease are the ovaries, the pelvic peritoneum, the cul-de-sac behind the uterus, the uterosacral ligament, and also the posterior surface of the uterus. The most common symptom is pelvic pain, which can be spontaneous, pain with menstruation or pain with intercourse. Other common symptoms are abnormal uterine bleeding, spotting prior to periods, and infertility.
Do these endometrial implants or endometriosis act like normal endometrium inside the uterus?
Not always. Endometrial implants can undergo cyclic histological changes similar to those found in normal endometrium. This shows that in most cases, ectopic endometrium is responding to hormonal changes that occur in the female every month. The endometrial tissue in endometriosis also undergoes atrophy after menopause, or after prescription of the medication that stops ovarian function.
However, the response is not similar in all cases. One reason for this discrepancy is the finding that estrogen receptors have been identified in a minority of endometriotic tissues. Another possible answer to the discordancy between normal endometrium and endometriosis and the apparent failure of drug therapy in some women is the lack of enzymes in endometriotic tissue for hormonal actions.
Why are ovaries the most common site of endometriosis?
If we accept the theory that retrograde menstruation is in large part responsible for the initiation of endometriosis in those women susceptible to the implantation of the endometrial cells, then the number one reason is the position of the ovary. The ovaries are adjacent to the opening of the tube in the pelvic area and that location alone will make the ovaries more prone to be contaminated with the regurgitated menstrual flow.
The other reason is that the ovaries have the highest level of steroid hormone compared to any other organ and hence they represent an ideal environment for implantation and growth of the endometrial tissue. In different studies, the involvement of the ovaries (either unilaterally or bilaterally) has been reported up to 75 percent of the time.
What is a chocolate cyst?
Ovarian endometriosis probably starts as a surface lesion. The process becomes invasive and the endometriotic lesion internalizes into the ovarian tissue. Once the menstrual flow and debris collect at the site of endometriosis in the ovaries, endometrial cysts form that are filled with chocolate-colored liquid. These are commonly called chocolate cysts, or endometriomA. These are nothing more than cysts which represent debris from prolonged cyclic menstruation in an enclosed areA. These cysts may sometimes attain impressive size, with some documented as large as a baseball or grapefruit that completely obliterate the normal ovary. However, usually there is a well-demarcated separation between the cyst wall and the normal adjacent ovarian tissue.
I was told that the changes in the peritoneal fluid due to endometriosis is one of the causes of my infertility. What does this mean?
Peritoneal fluid is the fluid which every person has in their abdominal cavity and which functions as a lubricant for the abdominal and pelvic organs. It has become apparent in the past decade or so that the presence of endometriosis is associated with changes in this peritoneal fluid, its volume, its cellular population and its biochemistry. Generally, it has been shown that the volume of the fluid is increased in women with endometriosis. The leukocytes have also been shown to be increased in number in the fluid of patients with endometriosis.
Also, the prostaglandin hormone concentration has been reported to be elevated in peritoneal fluid as well as the level of proteolytic enzymes which are all consistent with the localized inflammatory reaction around the endometriotic implants. Since these hormones could each alter the environment of the peritoneal fluid, which is in very close proximity to the ovaries and tubes, it can potentially alter their function. In recent studies, it has been shown that the peritoneal fluid in patients with endometriosis can act as a toxin to an embryo and may even stop the growth of the embryo in its early stages.
What are the most common sites of endometriosis in the pelvic area?
If we accept the theory of retrograde menstruation as the main cause for the initiation of endometriosis, the ovaries are the most frequently involved organ (in 75 percent of cases) because of the unique characteristics of their site. The next most common areas are the posterior cul-de-sac (70 percent of cases), the area between the uterus and the bowel, and the anterior fold of the uterus between the uterus and the bladder (35 percent of cases). Presumably, this is due to the effects of gravity. The next most common area is the posterior aspect of the pelvic wall and the uterosacral ligaments (35 percent) which are attached behind the uterus. The ureters are the most commonly affected pelvic organs also due to their site, which is again sitting close to the ovarian bed or opening of the tube to the pelvis. The next most common sites are the uterus (10 percent), the tubes, the sigmoid colon and the appendix. Due to high motility and active peristalsis, the small bowel is the least frequent organ involved in endometriosis (less than one percent).
What are the other common areas outside of the pelvis where we find endometriosis?
Endometriosis has been found in the appendix (2 - 5 percent of cases), large bowel (3 to 4 percent of cases) and the small bowel (less than one percent of cases). Much less frequently, we find endometriosis in the gall bladder, stomach, spleen and liver.
I was told that I have endometriosis on my incision where I had a Cesarean section. How is this possible?
At the time of a C-section, pieces of the uterine lining could be transplanted in the incision and start growing. In a recent study of 56 cases of endometriosis in surgical sites, almost half of the cases followed a C-section. These lesions cause local cyclical pain and, on occasion, even cyclical bleeding. Treatment is obviously surgical removal of the involved area.
What are pelvic adhesions? Why do people with endometriosis have adhesions?
Scarring of the peritoneum around endometriosis is a typical and very common finding. The explanation for this is that the bleeding that occurs around each menstrual cycle gets collected, and since there is no escape for this blood, it will start irritating the adjacent peritoneal surface, then start producing irritation and inflammation and eventually, scarring. These adhesions are most common in the immobile pelvic structures, and are most commonly found in the pelvic sidewalls, behind the uterus, between the sigmoid bowel or colon, and on the posterior aspect of the uterus and cervix.
If the retrograde flow of menstrual bleeding through the fallopian tube is a major mechanism for endometriosis, why don't all women have endometriosis?
Although some degree of menstrual backflow occurs almost universally, only those women who are predisposed to having endometriosis will allow the cells to implant in the pelvic area. Patients who have some deficiency in their immunological system, women who have more frequent periods (shorter than 27 days), or women who have longer days of bleeding with their period (more than 7 days) are more prone to develop endometriosis.
Is there any evidence that viable cells are in the menstrual flow?
Yes. The presence of viable endometrial cells in the menstrual flow has been demonstrated by culturing the menstrual flow and obtaining tissue cultures. Other evidence has been the presence of viable endometrial cells in the fallopian tube. Endometrial cells which have been obtained from the menstrual flow have been demonstrated to be plantable to other areas of the abdomen (i.e., the abdominal wall).
Other evidence supporting this theory is that endometriosis is extremely common at the site of the menstrual blood flow through the tube into the peritoneal cavity; for example, the pelvic sidewall next to or adjacent to the tube and the ovarian surface. Another interesting point is that the mobile pelvic structures, such as the bowel or fallopian tubes themselves, are less likely to allow attachment of transplanted endometrial cells, whereas fixed structures are anticipated and also have been shown to have a higher frequency of having these implants on them.
After reviewing all of these reasons, it becomes obvious that the preponderance of evidence suggests that endometriosis is a consequence of implantation of viable endometrial cells through the fallopian tubes at the time of menses..
Are there any other theories as to how endometriosis is developed besides this backflow theory?
Other theories for how endometriosis comes about include the following:
1. Spread of endometrial cells to other areas of the pelvis or other organs through the lymphatic channels.
2. Spread of endometrial cells through the blood vessels. The presence of many cases of endometriosis which have been reported in the lung, skin, thigh and extremities can be explained by this mode of transport.
3. Spread of endometrial cells through surgery. For example, at the time of cesarean section, some of the endometrial tissue can be spread or trapped in the abdominal wall and produce endometriosis in the future.
Are there any women who are more prone to have endometriosis?
Yes. Women in the reproductive age group are more prone to have endometriosis. Endometriosis is also common in women who have had uninterrupted cyclic menstruation for periods of more than five years. By this, I mean a woman who has had a period every month for five years which has not been interrupted by pregnancy. Endometriosis is less commonly seen in women with irregular cycles who are not ovulatory (not producing an egg), and in women who have stopped their regular cyclic period by any means such as pregnancy and lack of ovulation. Giving medication to produce pseudo-pregnancy or pseudo-menopause can stop the growth of endometriosis and give clinical improvement to the patient. Frequent pregnancies, especially those initiated early in the menstrual life (during the teen years), seem to insulate women against endometriosis, at least temporarily. Also, we have seen that endometriosis occurs more frequently in some families than in others.
How old is the disease?
Theoretically, endometriosis should have existed since the beginning of time. However, the first description was about 300 years ago and the first detailed description was in 1860 by a physician named Von Rokitansky.
Our modern-day understanding of endometriosis began with the pioneering efforts of a private physician named Sampson in Albany, New York, in the 1920s. Dr. Sampson proposed that the menstrual backflow through the tubes contained viable endometrial cells which could be transplanted to ectopic sites.